The 8-Minute Rule vs. Total Time Rule: A Guide to Accurate CPT Unit Billing for Therapy
Why can two therapists spend the same amount of time with a patient but still bill differently?
Why do some payers insist on counting every single minute whereas others focus only on the total session time?
These differences come from two important guidelines in therapy billing, i.e., the 8-minute rule and the total-time rule. One asks you to track time in small segments to decide how many billable units you can report, whereas the other looks at the whole session to determine the correct billing. As a result, understanding when each rule applies can be confusing, especially when insurers follow their own versions.
This blog breaks down both rules in the simplest way so you can avoid mistakes and bill with confidence.
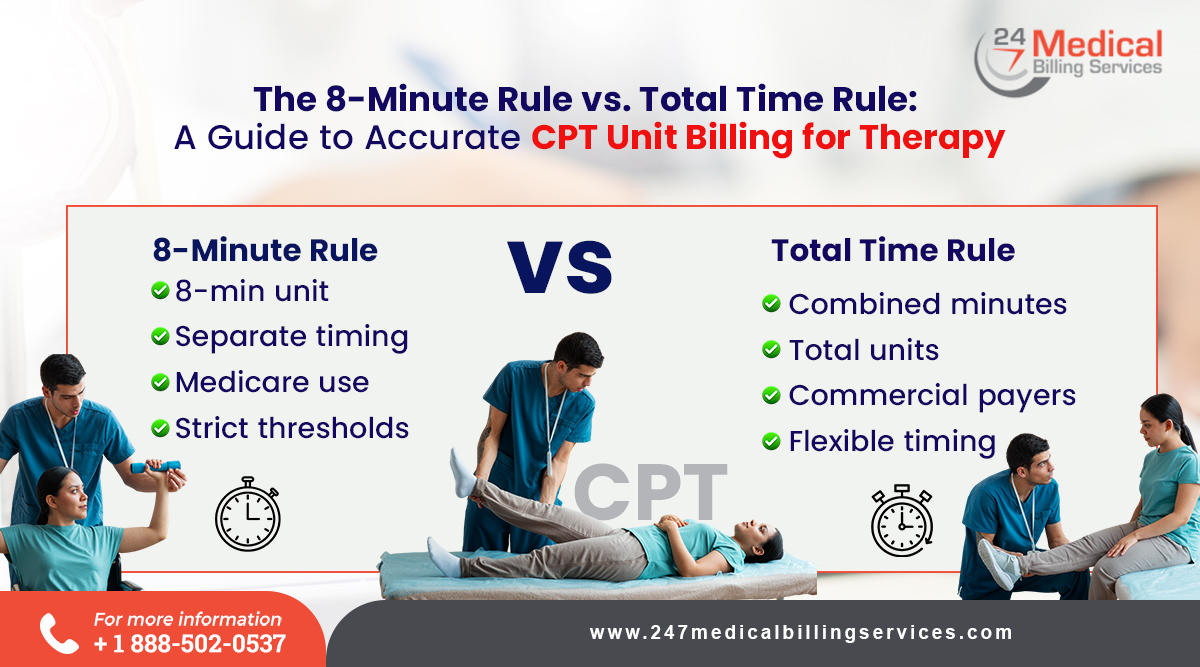
8-Minute Rule vs. Total Time Rule
The 8-minute rule and the total time rule are two different ways to count and bill time-based therapy services. Although both methods rely on the minutes a provider spends delivering skilled care, they follow different calculations.
-
Meaning
The 8-minute rule determines how many therapy units can be billed when a service is timed. It measures the minutes spent on each specific CPT code and allows providers to bill a unit once they reach at least eight minutes beyond a 15-minute block.
The total time rule considers the total minutes spent on all time-based services during the visit. Instead of reviewing each code separately, the rule combines all eligible minutes into a single total and uses that total to determine the correct units.
-
How is Time Counted?
The main difference lies in how each method measures time. The 8-minute rule checks the minutes attached to each code and requires individual tracking for every service. In contrast, the total time rule looks at the entire session and counts all timed minutes together. This difference influences documentation style and determines how carefully each code needs to be recorded.
-
Unit Calculation
The 8-minute rule calculates units by dividing minutes into 15-minute segments and adding a unit only when the remainder reaches eight minutes or more. Meanwhile, the total time rule converts the full session time into units without using a separate threshold for each service. This distinction affects how providers determine the final number of units they can bill.
-
Payer Policy Requirements
Another key difference is based on payer rules. Medicare and some Medicaid programs follow the 8-minute rule for outpatient therapy so providers must carefully track code-level minutes. However, many commercial insurers prefer the total time rule, which allows the minutes to be combined. Therefore, understanding the payer's method ensures that claims are submitted correctly and prevents billing errors.
-
Documentation Approach
Each rule also influences how documentation is prepared. Under the 8-minute rule, notes must show the time spent on each separate service to support the units billed. Under the total time rule, the focus is on the overall treatment time and the skilled tasks performed during the session. This difference shapes the structure of clinical notes and the details providers need to include.
-
Steps for Applying the Rule
The 8-Minute Rule:
Step 1: Identify Time-Based and Service-Based CPT Codes
You begin by reviewing all CPT codes used during the visit to determine which require time tracking. This helps you separate timed procedures from untimed services and ensures that only appropriate codes are included when calculating billable therapy minutes for the session.
Step 2: Record Minutes of Direct Skilled Therapy
You then document the exact minutes spent providing one-on-one, skilled therapeutic care. This step focuses solely on billable interactions with the patient excluding administrative duties and indirect tasks. Accurate time tracking ensures your documentation clearly reflects the proper amount of therapeutic work completed.
Step 3: Calculate the Total Timed Minutes
After recording minutes for each eligible service, you add them together to find the total amount of timed treatment provided. This combined number forms the basis for determining billable units. An explicit total ensures your calculations are consistent, organized and aligned with the time rules you must follow.
Step 4: Convert the Total Minutes into Units
You convert the total time in minutes into units by dividing it into 15-minute segments. This method establishes a standardized approach to assigning units and helps you maintain a consistent billing structure. It also ensures your calculations remain transparent and easy for payers to understand.
Step 5: Apply the 8-Minute Threshold
Once the units are complete, you count the leftover minutes. If these remaining minutes reach eight or more, you may add an additional billable unit. This step ensures any meaningful extra time spent providing therapy is included, supporting accurate reimbursement for the care delivered.
Step 6: Assign Units to the Correct CPT Codes
Finally, you distribute the total calculated units among the specific CPT codes used during the session. The last unit must be assigned to a code with at least eight documented minutes, ensuring compliance with the rule and maintaining accuracy across all billed services.
The Total Time Rule:
Step 1: Check the Payer’s Time Calculation Method
You begin by reviewing the payer's guidelines to understand how they expect treatment time to be calculated. Some use simple time-based billing whereas others use block-based billing. In fact, knowing this information early ensures your documentation and unit calculations match the payer's expectations from the start.
Step 2: Determine Whether Time Can Be Combined
Next, confirm whether the payer allows combining minutes from different timed services. This step shapes how you document the session and influences how you report your total minutes. In fact understanding this requirement helps you avoid errors and ensures your billing remains consistent with their policy.
Step 3: Document All Billable Minutes Accurately
You then record the complete total time spent delivering skilled therapeutic care. This documentation must clearly reflect all billable actions performed during the visit. Accurate time entries support medical necessity, create a clear treatment record, and help ensure your billing aligns fully with payer expectations.
Step 4: Calculate Units Based on Payer Policy
After documenting the total time, convert those minutes to the correct number of units using the payer's required calculation rules. This may involve block-based billing or straight conversions. Therefore, following their method ensures your claim is correct, consistent and less likely to be delayed or denied.
Step 5: Ensure Documentation Matches the Billed Units
Finally, you review your notes to confirm your documented minutes support the units billed. This step strengthens compliance, prevents discrepancies and reduces the chance of audits or claim issues. In fact, clear alignment between documentation and billing helps maintain accurate, reliable and payer-ready clinical records.
Conclusion
Although the 8-minute rule and the total-time rule serve similar purposes, they apply in different billing situations. This means that each requires a separate approach for recording minutes, assigning units and meeting insurer expectations. As payers often change their requirements, clinical teams can quickly find the process confusing and demanding. Thereby outsourcing these tasks to 24/7 Medical Billing Services becomes a practical and dependable solution. Their experts identify which rule applies in every scenario, interpret payer guidelines correctly and ensure that all time logs and unit calculations follow the proper method. They also handle documentation checks and claim submissions with consistent accuracy. Therefore, your practice can reduce errors, strengthen compliance, and gain more time to focus on providing high-quality care to your patients.
FAQs
Can the same therapy session be billed differently under different payers?
Yes, as each insurer may apply a different rule for counting time and units.
Are non-timed services affected by these rules?
No, only time-based codes are linked to the 8-minute or total-time rule.
Can therapists mix both rules in a single claim?
No, the payer’s rule determines which method must be followed for that claim.


.png)
