Billing Chronic vs. Acute Wounds: ICD-10 Linkage Mistakes to Avoid
Why do two wounds that look similar at the bedside create completely different challenges in medical billing?
What makes chronic wounds demand detailed and condition-specific coding whereas acute injuries rely on precise encounter-level documentation?
How can providers avoid costly denials by understanding these distinctions early?
As payers tighten rules and documentation scrutiny increases, decoding the difference between billing chronic and acute wounds has become essential for accurate reimbursement. This blog explores these differences clearly and helps providers strengthen their wound care billing approach.
Billing Chronic vs. Acute Wounds
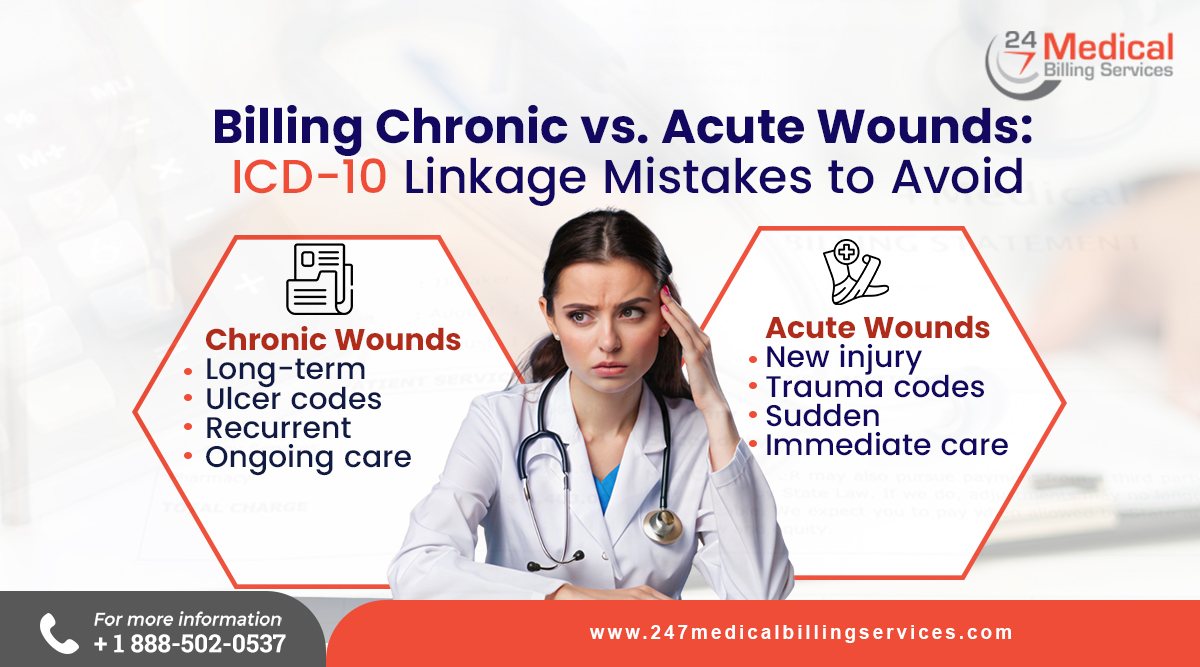
Billing chronic and acute wounds requires understanding how payers classify, verify and reimburse these services based on medical necessity and documentation. Chronic wounds usually need ongoing care with structured clinical records, whereas acute wounds involve short-term treatment of injuries or surgical openings.
-
Difference in Coding Requirements
Chronic wounds are coded using diagnosis codes that indicate the cause, site, and stage, which help the payer confirm the long-term medical need. Acute wounds rely on injury or procedure-related diagnosis codes that reflect the immediate condition. Using the correct ICD-10 code ensures the claim matches the clinical story and supports compliant billing.
-
Selecting the Correct CPT or HCPCS Procedure Code
Billing chronic wounds often requires CPT codes for active wound care, selective debridement or advanced therapies that involve repeated visits. Acute wound billing usually uses repair or closure codes that describe the one-time procedure performed. In fact, choosing the correct procedure code ensures that payment reflects the actual work and complexity of the service.
-
Documentation Standards for Both Wound Types
Chronic wound documentation must include measurements, tissue descriptions, previous responses to treatment, and evidence of ongoing need. Acute wound documentation needs to show what caused the wound and how the provider assessed and treated it on that date. Thereby, complete and clear notes help the payer understand the rationale behind the billed codes.
-
Rules on Bundling and Reporting Services Correctly
Payers often bundle certain wound care services, so chronic wound billing must follow rules that prevent reporting multiple procedures on the same site when they are considered inclusive. Acute wound billing also requires checking if closure, cleaning, and certain supplies are already included in the primary procedure code. Therefore, reviewing bundling guidance reduces the risk of denials.
-
Use of Modifiers
Chronic wound claims may need modifiers to show distinct services, separate sites or a valid evaluation and management visit on the same day. Acute wound claims may also use modifiers when multiple injuries or procedures are treated during one encounter. As a result applying modifiers correctly helps differentiate services and supports appropriate reimbursement.
-
Frequency Limits and Prior Authorization
Chronic wound care often has frequency limits set by payers, so claims must reflect medically necessary, continued improvement or clinical justification. Acute wound treatment rarely requires prior authorization unless advanced techniques are used. Thereby, checking payer rules ahead of time prevents issues during claim review.
ICD-10 Linkage Mistakes to Avoid
Avoiding ICD-10 linkage errors is essential for accurate billing, especially when distinguishing chronic and acute wounds. In fact, proper code selection depends on precise documentation, correct sequencing, and matching diagnosis codes to the procedures performed.
-
Using Unspecified Codes when Details are Available
Coders often select unspecified ICD-10 codes even though the documentation provides clear information about wound location, laterality, stage or underlying cause. But choosing a more precise code is vital as payers rely on this detail to confirm medical necessity. As a result, the claim becomes stronger and more accurate when specificity from the medical record is fully captured.
-
Sequencing Acute and Chronic Conditions Incorrectly
When a provider documents a wound as both acute and chronic, ICD-10 guidelines require listing the acute condition first. But placing the chronic code before the acute code violates sequencing rules and creates inconsistencies during claim review. Therefore, correct sequencing helps the payer understand the patient's condition trajectory and validates the rationale for treatment.
-
Assuming Acuity Without Provider Confirmation
Coders should never decide whether a wound is acute, chronic, or a combination based on the length of treatment or clinical patterns. Only the provider can determine the acuity and must document it clearly. As a result, coding without explicit provider wording leads to assumptions that may misrepresent the condition and result in claim disputes.
-
Using History Codes for Active Wounds
"History of" codes apply to past or resolved conditions, so assigning them to an active wound is inaccurate. Coders must confirm that the wound is currently being evaluated or treated and select an active diagnosis code accordingly. Using the appropriate code ensures the claim reflects the actual clinical situation and justifies the billed services.
-
Mismatch Between Diagnosis and Procedure Codes
Each wound care procedure requires a diagnosis that accurately explains why the service was needed. In fact, payers often question the claim when the depth, severity, or type of wound in the clinical record does not match the diagnosis linked to the procedure. Therefore, proper linkage strengthens medical necessity and supports reimbursement for the documented work.
-
Confusing Chronic Ulcers With Traumatic Injuries
Chronic ulcers and traumatic injuries fall under different ICD-10 code categories that represent distinct clinical situations. In fact, the selection of an injury code for a chronic ulcer or using an ulcer code for an acute wound creates a mismatch that can delay or reduce payment. As a result, accurate classification ensures the diagnosis aligns with the documented wound type.
-
Not Reporting the Underlying Condition When Required
Many wounds develop as a result of systemic diseases such as diabetes or venous insufficiency. Thereby, the underlying condition should be coded first to reflect the complete clinical picture when documentation shows this connection. Therefore, correct sequencing helps payers understand why the wound persists and supports the need for ongoing or advanced wound care services.
-
Using Outdated or Invalid ICD-10 Codes
ICD-10 codes are updated annually, so using outdated or deleted codes can result in immediate claim rejections. As a result, practices should ensure their billing systems and coding references match the current code set. In fact, regular code updates help maintain accuracy and prevent delays caused by outdated information in electronic health records or charge-capture tools.
-
Missing the Required Seventh Character for Injury Codes
Some injury codes require a seventh character to indicate whether the encounter is initial, subsequent or due to complications. It is important to note that leaving out this character makes the code incomplete and therefore invalid for billing. As a result, the healthcare provider needs to ensure that the correct character is applied as it helps clarify the stage of care and supports proper claim adjudication.
-
Inaccurate Coding Due to Insufficient Documentation
Claims are often denied when the documentation lacks key details such as wound size, depth, tissue type, or treatment history. Coders rely entirely on provider notes to create accurate claims, so missing information directly affects code selection. Therefore, complete documentation enables the coder to assign precise ICD-10 codes that accurately reflect the clinical scenario.
Outsourcing Wound Care Billing and Coding Services
Outsourcing wound care billing and coding offers providers a unified, streamlined solution that removes administrative pressure and ensures precise handling of chronic and acute wound claims. A dedicated billing partner such as 24/7 Medical Billing Services manages every component of the process, from accurate code selection to timely claims submission and continuous denial follow-up to allow clinicians to focus entirely on patient care. In fact, such experienced teams stay current with payer updates, documentation expectations, and code revisions which reduces compliance risks and prevents costly errors that often arise in-house. This approach delivers reliability, efficiency, and financial stability, making it an end-to-end solution for practices seeking accuracy and improved revenue performance in wound care billing.
FAQs
Do payers require images for wound claims?
Some payers request wound images as supplemental proof of medical necessity.
Are wound debridement codes frequently audited?
Yes, they face frequent audits due to scrutiny of medical necessity.
Do payers limit the frequency of billed wound procedures?
Yes frequency edits apply to ensure procedures are not billed too often.


.png)
