Mental Health CPT Codes: Essential Billing Reference for Psychiatrists & Therapists
In 2025, the mental health sector is experiencing a significant transformation, driven by advancements in telehealth and digital therapeutics. Telehealth services now account for approximately one-third of all behavioral health visits, a substantial increase from just 1% in 2019. This shift has led to the introduction of new CPT codes, such as G0553 and G0554, to accommodate digital mental health treatments.
Moreover the integration of behavioral health into primary care settings is gaining momentum with initiatives like same-day billing for mental health and primary care services being implemented to streamline patient care.
These developments highlight the necessity for mental health professionals to stay abreast of the latest CPT code updates and billing practices to ensure accurate reimbursement and compliance. This blog aims to provide psychiatrists and therapists with a comprehensive understanding of the most commonly used mental health CPT codes in 2025.
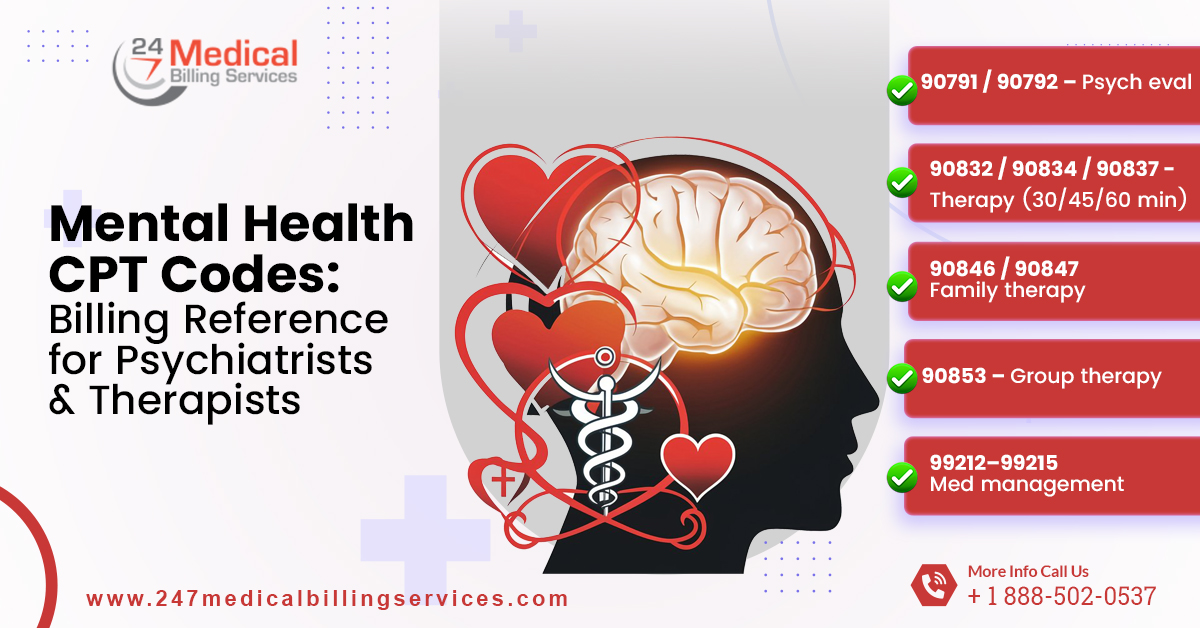
Commonly Used Mental Health CPT Codes (2025)
Accurate coding ensures proper reimbursement, maintains compliance, and reflects the exact services provided. The following are the most commonly used mental health CPT codes--
1. Diagnostic Evaluations
- 90791 – Psychiatric Diagnostic Evaluation (without medical services):
This code is used for initial assessments that evaluate a patient’s mental health condition without providing medical services, such as prescribing medications.
- 90792 – Psychiatric Diagnostic Evaluation (with medical services):
This code applies when a psychiatrist conducts an evaluation that includes medical services such as medication management or monitoring the effects of treatment.
2. Psychotherapy Sessions
- 90832 – Psychotherapy, 30 minutes:
This code is used for sessions lasting 16 to 37 minutes and covers brief therapy aimed at addressing immediate emotional or behavioral concerns.
- 90834 – Psychotherapy, 45 minutes:
This code applies to sessions of 38 to 52 minutes to provide moderate-length therapy for structured interventions and emotional support.
- 90837 – Psychotherapy, 60 minutes:
This code is for sessions lasting 53 minutes or more, which is suitable for comprehensive therapy or more complex patient needs requiring extended time.
3. Family and Couples Therapy
- 90846 – Family or couples psychotherapy (without patient present):
This code is used when therapy involves family members or partners, but the primary patient is not present, focusing on family dynamics and communication patterns.
- 90847 – Family or couples psychotherapy (with patient present):
This code applies when the patient participates with family members or partners to address relational issues and collaborative treatment strategies.
4. Group Therapy
- 90853 – Group psychotherapy (other than of a multiple-family group):
This code covers therapy provided to multiple patients in a group setting to focus on shared therapeutic goals and peer support.
5. Crisis Intervention
- 90839 – Psychotherapy for crisis (first 60 minutes):
This code is used for intensive sessions that address acute mental health crises lasting up to 60 minutes to focus on immediate stabilization and intervention.
- 90840 – Psychotherapy for crisis (each additional 30 minutes):
This add-on code is billed in conjunction with 90839 when crisis sessions extend beyond the initial 60 minutes to ensure proper documentation and reimbursement.
6. Interactive Complexity
- +90785 – Psychotherapy with interactive complexity:
This add-on code is applied when sessions involve additional challenges, such as communication barriers, interpreters or complex dynamics, and is billed in conjunction with primary psychotherapy codes.
7. Telehealth Services
- 98000–98003 – New client audio-video telemedicine visits:
These codes are used for telehealth sessions with new clients, conducted via audio-video technology, to enable a comprehensive assessment and therapy to be provided remotely.
- 98004–98007 – Established client audio-video telemedicine visits:
These codes apply to telehealth sessions for returning clients conducted via audio-video technology to support ongoing therapy and treatment.
- 98008–98011 – New client audio-only telemedicine visits:
These codes cover telehealth sessions with new clients conducted via audio-only technology to enable assessment and counseling without video.
- 98012–98015 – Established client audio-only telemedicine visits:
These codes are used for audio-only telehealth sessions with returning clients for maintaining continuity of care remotely.
- 98016 – Brief virtual check-in encounter:
This code is used for short telehealth encounters to monitor progress or provide brief guidance which typically lasts only for a few minutes.
8. Behavioral Health Integration (BHI)
- 99492 – Care coordination for behavioral health integration (first 60 minutes):
This code is used for the initial 60 minutes of care coordination in integrated behavioral health, including treatment planning and communication with providers.
- 99493 – Care coordination for behavioral health integration (each additional 30 minutes):
This code applies to each additional 30 minutes of ongoing care coordination beyond the first hour to ensure proper documentation and billing.
- 99494 – Care coordination for behavioral health integration (each additional 60 minutes):
This code is used when an additional 60 minutes of BHI care coordination is required to support complex cases and extended planning.
- G2214 – Care coordination for behavioral health integration (each additional 30 minutes):
This code covers an additional 30 minutes of BHI care coordination beyond the standard session to emphasize ongoing management and patient support.
Guidelines for Use of Correct Mental Health CPT Codes
Proper use of mental health CPT codes is crucial for delivering accurate billing, maintaining regulatory compliance and documenting clinical care effectively. In fact, adhering to structured guidelines allows providers to streamline billing, reduce claim denials and improve overall practice efficiency.
- Understand Mental Health CPT Codes
Mental health providers should familiarize themselves with all relevant CPT codes including diagnostic evaluations and individual psychotherapy as correct identification ensures accurate billing and compliance.
- Match Code to Session Type
Always select the CPT code that corresponds precisely to the type of session provided, whether it is individual, family, couples, group or crisis therapy. Accurate coding reflects the services delivered and supports healthcare reimbursement.
- Match Code to Session Duration
Choose codes based on the exact session duration, such as 30, 45, or 60 minutes for psychotherapy, or time-based codes for crisis or add-on services. Accurate time coding prevents underpayment or overbilling.
- Use Add-On Codes Appropriately
Apply add-on codes like +90785 for interactive complexity, +90840 for extended crisis therapy, and BHI codes (99492, 99493, 99494, G2214) only when medically necessary, as correct use ensures proper reimbursement for complex or additional services.
- Maintain Detailed Documentation
Session notes must include the date, time, duration, diagnosis, treatment plan, therapeutic techniques, and patient progress, while also supporting add-on, crisis, or telehealth codes.
- Follow Telehealth Coding Rules
Telehealth codes for audio-video or audio-only sessions should be applied correctly for both new and established clients, including brief virtual check-ins, while maintaining documentation standards identical to those for in-person visits.
- Ensure Compliance and Audit Readiness
Following AMA, payer, and regulatory guidelines consistently, while maintaining detailed documentation, ensures compliance and audit readiness, as proper coding supports billed services and prevents reimbursement disputes or penalties.
Consider Outsourcing Mental Health Billing
Outsourcing mental health billing proves to be an optimal solution for practices aiming to improve financial performance and operational efficiency. Specialized billing services such as 24/7 Medical Billing Services possess in-depth knowledge of complex CPT codes, payer-specific requirements, and evolving regulations, ensuring accurate and timely reimbursements. For instance, practices billing over $100,000 monthly have reported a 5 - 15% increase in collection rates through these professional billing services which translates to substantial annual revenue gains
Moreover, these services provide real-time reporting and analytics to enable providers to monitor revenue trends, identify potential issues, and make informed financial decisions. This proactive approach not only enhances cash flow but also supports strategic planning and growth. Additionally, outsourcing helps maintain compliance with ever-changing regulations, such as the expanded coverage for telehealth services under Medicare, which mandates equal reimbursement for mental health services.
FAQs
Q1. Are CPT codes the same for inpatient and outpatient therapy?
No, specific codes apply depending on the treatment setting.
Q2. Can a single session include multiple CPT codes?
Add-on codes or combined services may be billed with proper documentation.
Q3. Are CPT codes required for self-pay patients?
They help create a clear superbill for potential insurance claims.


.png)
